Overview
Bleeding is a common problem in cancer patients. It can happen for different reasons, such as the cancer invading blood vessels or the effects of cancer treatments.
Certain medications can also make bleeding worse.
Let us explore some possible causes of bleeding in cancer patients:
Low Platelet Count (Bleeding)
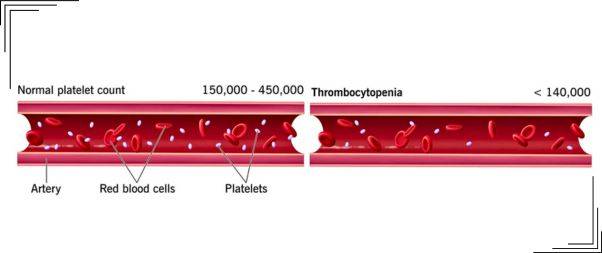 Platelets are special blood cells that help your blood to clot and stop bleeding. When the number of platelets in your blood is lower than normal, it is called a low platelet count or Thrombocytopenia.
Platelets are special blood cells that help your blood to clot and stop bleeding. When the number of platelets in your blood is lower than normal, it is called a low platelet count or Thrombocytopenia.
Having a low platelet count means that your blood doesn’t clot properly, which increases the risk of excessive bleeding.
The lower your platelet count, the higher the risk of bleeding. Your doctor will determine what level of platelet count is considered low.
If your platelet count is very low, your doctor may postpone or reduce your treatment. To measure your platelet level, your doctor will use a blood test called a complete blood count (CBC).
Causes of Bleeding
Bleeding is a common problem for patients with advanced cancer. About 10% of all cancer patients experience at least one episode of bleeding, and the number increases to almost 30% in patients with blood-related cancers.
The severity of bleeding can vary, ranging from minor oozing to major or even life-threatening bleeds.
There are several factors that can contribute to bleeding in cancer patients.
Specific types of cancer: Patients with lymphomas or leukemias may have a higher likelihood of experiencing bleeding.
Certain cancer treatments: Chemotherapy or radiation therapy, particularly when administered in high doses or in combination with other chemotherapy drugs, can lead to a decrease in platelet levels. Immunotherapies, certain pain-relieving drugs (NSAIDs), and blood thinners (anticoagulants) commonly used in cancer patients can make bleeding worse.
Antibody-related destruction: In some cases, antibodies in the body may mistakenly attack and destroy platelets, resulting in bleeding.
Other health issues or medications: Apart from cancer-related factors, additional health conditions or medications unrelated to the cancer can also contribute to a decrease in platelet count.
Tumor growth and invasion: Cancer cells can infiltrate and damage blood vessels, leading to bleeding. As tumors grow, they can invade nearby blood vessels, causing them to rupture and resulting in bleeding.
Ulceration or erosion of tumors: Some tumors, particularly those in the gastrointestinal tract, may develop ulcers or erosions on their surface. These areas can be prone to bleeding, leading to blood loss.
Disseminated intravascular coagulation (DIC): DIC is a condition in which the blood’s normal clotting process becomes overactive and leads to the formation of small blood clots throughout the body. This can deplete the body’s clotting factors and platelets, increasing the risk of bleeding.
Organ dysfunction: In advanced stages of cancer, the disease can affect the normal functioning of organs, such as the liver or kidneys. Impaired liver function can lead to a decrease in clotting factors, while kidney dysfunction may result in abnormalities in the blood’s composition and clotting ability.
It’s important to consult with your doctor to understand the specific causes of your low platelet count and to determine appropriate treatment options.
Challenges in Studying and Treating Bleeding
There is limited research on treatments to manage bleeding in patients with advanced cancer, and no randomized therapeutic trials have been conducted.
Conducting such trials is challenging due to the complex nature of the patient population, the involvement of multiple medical specialties, and the various sites affected by bleeding.
Existing studies often focus on a single treatment method, and there is no consistent definition of bleeding or standardized evaluation of treatment response.
Moreover, the available literature relies heavily on retrospective studies, making it difficult to establish uniform definitions and evaluation methods for outcomes.
Available Treatments
There are several available treatments to stop bleeding in cancer patients, depending on the underlying cause and severity of the bleeding.
Here are some commonly used interventions:
Platelet transfusion: If the bleeding is due to a low platelet count (thrombocytopenia), transfusing platelets can help increase the platelet levels and promote clotting.
Medications to promote clotting: Certain medications, such as desmopressin or clotting factors, may be administered to enhance the blood’s ability to clot and control bleeding.
Local measures:
- Directly applying pressure to the bleeding site can help stop bleeding or reduce its intensity.
- Using specialized dressings or bandages can help promote clotting and provide compression to stop bleeding.
- In some cases, packing the bleeding site with special materials can help control bleeding and promote clot formation.
- Applying topical agents, like thrombin or fibrin glue, to the bleeding site can aid in clot formation.
Interventional procedures:
- Embolization: This procedure involves the insertion of small particles or a special substance into the blood vessels supplying the bleeding site to block the blood flow and stop bleeding.
- Endoscopic procedures: Using an endoscope, a flexible tube with a camera, doctors can directly visualize and treat bleeding areas within the gastrointestinal tract or other accessible organs.
- Surgical treatment: In severe cases or when other interventions are ineffective, surgical procedures may be necessary to stop bleeding. This can involve removing the bleeding tissue, repairing blood vessels, or other appropriate surgical interventions.
Conclusion
Bleeding is a significant concern for patients with advanced cancer. The causes of bleeding can be multifactorial, including cancer-related factors, treatment effects, and low platelet levels.
However, research on effective palliative treatments for bleeding in advanced cancer is limited, and there is a need for further studies to better understand and manage this issue.
Also Read







