Dementia is a broad term that includes different diseases and conditions affecting how we think, remember, make decisions, and even behave.
When someone has dementia, their mental abilities decline, which can make it hard to do everyday things.
Research shows that around half of people aged 85 and above have some form of dementia. While current medications can slow down the worsening of cognitive problems, we still need better treatments to help people with dementia.
What is Dementia?
Dementia is a term used to describe a decline in mental function, and it’s not a specific disease itself.
When someone has dementia, their mental abilities decrease from a higher level they had before. This decline is significant enough to interfere with their daily life.
People with dementia experience difficulties in various areas, including:
- Memory
- Reasoning
- Language
- Coordination
- Mood
- Behavior
Dementia occurs when certain parts of the brain responsible for learning, memory, decision-making, or language are affected by diseases or infections.
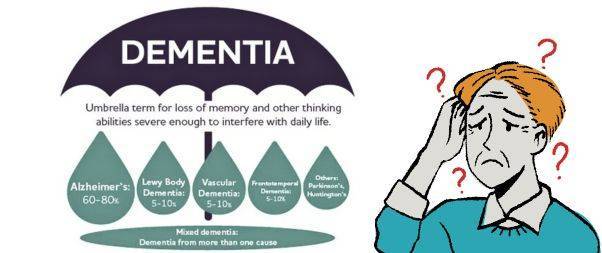
The most common cause of dementia is Alzheimer’s disease.
However, there are other known causes of dementia, including:
- Vascular dementia
- Dementia with Lewy bodies
- Frontotemporal dementia
- Mixed dementia
- Dementia due to Parkinson’s disease
- Dementia-like conditions caused by reversible factors such as medication side effects or thyroid problems.
Signs and Symptoms
In some cases, changes in mood and behavior can occur even before memory problems become apparent. As dementia progresses, symptoms worsen, and most individuals will require assistance with daily activities.
Early signs and symptoms of dementia may include:
- Forgetting recent events or things
- Misplacing or losing items
- Getting lost while walking or driving
- Feeling confused, even in familiar places
- Losing track of time
- Difficulties in problem-solving or decision-making
- Struggling with conversations or finding the right words
- Facing challenges in performing familiar tasks
- Misjudging distances visually
Common changes in mood and behavior can include:
- Anxiety, sadness, or frustration related to memory loss
- Personality changes
- Engaging in inappropriate behaviors
- Withdrawing from work or social activities
- Decreased interest in other people’s emotions
Dementia affects each person differently, depending on the underlying causes, existing health conditions, and the individual’s cognitive function prior to the onset of the illness.
Most symptoms tend to worsen over time, although some may disappear or only manifest in later stages of dementia.
As the disease progresses, individuals often require increased assistance with personal care. They may struggle to recognize family members or friends, experience difficulty in mobility, lose control over bodily functions such as bladder and bowel movements, encounter challenges related to eating and drinking, and exhibit behavior changes like aggression that can be distressing for both the person with dementia and those around them.
Who is Affected by Dementia?
Dementia is primarily observed in older individuals, making it a late-life disease.
Approximately 5% to 8% of people aged 65 and above have some form of dementia, and this percentage doubles every five years beyond that age. It is estimated that up to half of individuals aged 85 and older experience dementia.
The prevalence of Alzheimer’s disease and related dementias among different racial groups in the population aged 65 and older is as follows:
- Blacks: 14%
- Hispanics: 12%
- Non-Hispanic whites: 10%
- American Indian and Alaska Natives: 9%
- Asian and Pacific Islanders: 8%
These statistics provide insights into the impact of dementia across various racial and ethnic backgrounds within the older population.
How Common is Dementia?
According to the U.S. Centers for Disease Control and Prevention (CDC), approximately 5 million adults aged 65 or older in the United States are currently living with Alzheimer’s disease and related forms of dementia.
Looking ahead, the CDC projects that by the year 2060, the number of people affected by dementia will reach around 14 million, accounting for approximately 3.3% of the population.
Alzheimer’s disease specifically ranks as the sixth leading cause of death in the United States, and it is the fifth leading cause of death among individuals aged 65 and older.
These statistics highlight the significant impact that dementia has on individuals, families, and society as a whole.
Does Memory Loss mean Dementia is Starting?

There is a common misconception that memory loss automatically indicates the onset of dementia. However, memory loss can have various causes, and experiencing memory difficulties does not necessarily confirm a dementia diagnosis.
It is important to recognize that certain memory changes are a normal part of aging. As we grow older, some neurons in our brain naturally decline. However, this type of age-related memory loss is not severe enough to significantly impact daily functioning.
Dementia, on the other hand, goes beyond ordinary forgetfulness. It affects a person’s ability to function effectively. Dementia is not simply misplacing keys; it can involve forgetting the purpose of keys altogether. It’s crucial to understand that dementia is not a normal aspect of aging.
It’s essential to differentiate between occasional memory lapses, which can happen to anyone, and persistent memory problems that disrupt daily life. If you or a loved one are concerned about memory loss or cognitive decline, it’s important to consult with a healthcare professional for proper evaluation and diagnosis.
Diagnosing Dementia
Diagnosing dementia can be a complex task as there are various diseases and conditions that can contribute to its development. Moreover, many of the symptoms associated with dementia overlap with those of other illnesses.
To determine whether dementia is the underlying cause of cognitive decline, your healthcare provider will undertake several steps:
- Assessing symptom progression: Your healthcare provider will inquire about the pattern and progression of your symptoms to understand how they have evolved over time.
- Reviewing medical history: A comprehensive understanding of your medical history is crucial. Your healthcare provider will gather information about your past illnesses, medications, and family history, particularly related to dementia.
- Conducting tests: Several tests may be ordered to assist in the diagnostic process, including laboratory tests, imaging tests, and neurocognitive assessments.
- Laboratory tests: These tests aim to rule out other possible causes of dementia symptoms, such as infections, inflammation, thyroid problems, or vitamin deficiencies.
- Imaging tests: Brain imaging techniques like computed tomography (CT) or magnetic resonance imaging (MRI) can provide detailed images of the brain, helping to identify abnormalities such as stroke, bleeding, tumors, or fluid accumulation.
- FDG-PET scan: In certain cases, a specialized brain scan known as FDG-PET may be recommended to evaluate brain function and assess cognitive decline.
- Neurocognitive testing: Through written and computerized tests, healthcare providers assess various mental abilities including problem-solving, learning, memory, judgment, planning, reasoning, language, and more.
- Psychiatric evaluation: A mental health professional may be involved to evaluate factors like depression, mood changes, or other psychiatric conditions that could contribute to memory loss.
Neurologists and geriatricians often play a crucial role in the diagnostic process, combining their expertise to arrive at an accurate diagnosis.
It’s important to remember that diagnosing dementia requires a comprehensive evaluation and collaboration among healthcare professionals, and the process may take time to ensure an accurate assessment of the condition.
Treatment
When discussing dementia, it’s important to clarify the terms “treatable,” “reversible,” and “curable.” While all or most forms of dementia are considered treatable, meaning that medications and other measures can help manage symptoms, it’s crucial to note that most types of dementia cannot be cured or fully reversed.
Treatment options typically provide modest benefits.
However, there are certain forms of dementia that can be successfully reversed when caused by treatable underlying factors. These dementia-like symptoms may result from:
- Side effects of medications, illicit drugs, or alcohol
- Removable tumors
- Subdural hematoma (blood accumulation beneath the brain’s outer covering caused by head injury)
- Normal pressure hydrocephalus (excessive cerebrospinal fluid buildup in the brain)
- Metabolic disorders, such as vitamin B12 deficiency
- Hypothyroidism (low levels of thyroid hormones)
- Hypoglycemia (low blood sugar)
- Depression
Even when dementia is not reversible, there are medications available that can partially address memory loss and behavioral issues associated with certain forms of dementia. These include:
- Alzheimer’s disease
- Multi-infarct (vascular) dementia
- Dementias related to Parkinson’s disease and similar conditions
- AIDS dementia complex
- Creutzfeldt-Jakob disease
While treatment options can help manage symptoms and improve quality of life, it is important to acknowledge that they do not provide a complete cure for dementia. Each case is unique, and treatment plans are tailored to individual needs and circumstances.
It is crucial to consult with healthcare professionals to receive an accurate diagnosis, discuss treatment options, and develop a personalized care plan for managing dementia symptoms.
Self Care with Dementia

If you have been diagnosed with dementia, there are several self-care strategies that can help you manage your symptoms and improve your overall well-being:
- Stay physically active: Engage in regular physical activity that suits your abilities and interests. It can be as simple as taking walks, doing light exercises, or participating in activities like yoga or tai chi.
- Eat healthily: Maintain a balanced diet rich in fruits, vegetables, whole grains, and lean proteins. Proper nutrition is vital for brain health and overall well-being.
- Stop smoking and drinking alcohol: If you smoke or consume alcohol, consider quitting or reducing your intake. Both smoking and excessive alcohol consumption can worsen symptoms and have negative effects on your health.
- Regular check-ups: Schedule regular visits with your doctor to monitor your overall health and address any concerns or changes in your condition.
- Use memory aids: Help manage memory difficulties by writing down important tasks, appointments, and reminders. Utilize calendars, sticky notes, or smartphone apps to assist you in staying organized.
- Engage in enjoyable activities: Continue pursuing hobbies and activities that bring you joy and fulfillment. Participating in activities that stimulate your mind and provide a sense of purpose can be beneficial.
- Stay connected: Maintain social connections with friends, family, and your community. Engaging in social interactions and participating in community life can help improve your emotional well-being.
- Plan ahead: As dementia progresses, it may become challenging to make important decisions for yourself or manage your finances. Consider the following steps:
- Identify trustworthy individuals who can support you in decision-making and help you communicate your preferences.
- Create an advance plan outlining your care and support preferences, ensuring your wishes are known and respected.
- Carry identification with your address and emergency contact information whenever you leave the house.
- Seek support: Reach out to family, friends, and support groups for assistance. Communicate your needs and concerns, and don’t hesitate to ask for help when needed.
- Take care of yourself as a caregiver: If you are providing care and support for someone with dementia, remember to prioritize your own well-being. Seek assistance from others, take regular breaks, and practice stress management techniques. Consider joining support groups or seeking professional guidance to navigate the challenges of caregiving.
By implementing these self-care strategies, you can enhance your quality of life and better manage the impact of dementia on your daily life.
Risk Factors
Several factors can increase the risk of developing dementia. It’s essential to be aware of these risk factors to better understand the potential for developing the condition:
- Age: Age is the most significant risk factor for dementia. The likelihood of developing dementia increases as you grow older, with the majority of cases affecting individuals over the age of 65.
- Family History: Having a family history of dementia, particularly among biological parents or siblings, can increase your own risk of developing the condition. Genetic factors can play a role in certain types of dementia.
- Down Syndrome: Individuals with Down syndrome are at a higher risk of developing early-onset Alzheimer’s disease during middle age. The presence of an extra chromosome 21 in individuals with Down syndrome contributes to this increased risk.
- Poor Heart Health: Poor cardiovascular health, characterized by conditions like high cholesterol levels, high blood pressure, atherosclerosis, and smoking, can raise the risk of dementia. These conditions, along with diabetes, impact blood vessels, potentially leading to reduced blood flow and an increased likelihood of strokes.
- Race and Ethnicity: Studies indicate that certain racial and ethnic groups may have a higher risk of developing dementia. Black individuals have double the risk compared to white individuals, while Hispanic individuals are 1.5 times more likely to develop dementia than their white counterparts.
- Brain Injury: Experiencing a severe brain injury can increase the risk of developing dementia. Traumatic brain injuries, such as those resulting from accidents or falls, can have long-term effects on cognitive function.
It’s important to note that having one or more risk factors does not guarantee the development of dementia. Risk factors indicate an increased likelihood but do not provide a definitive prediction.
Many factors contribute to the complex nature of dementia, and additional research is continually being conducted to further understand the risk factors involved.
By being aware of these risk factors, individuals can make informed decisions about their lifestyle, take appropriate preventive measures, and seek early medical intervention if necessary.
When to Seek Medical Advice for Dementia Concerns

If you or your loved ones notice any of the following changes, it is advisable to schedule an appointment with your healthcare provider:
- Memory: Significant changes in memory, such as forgetting important information, struggling to recall recent events or conversations, or relying heavily on reminders and notes.
- Mental Functioning: Noticeable decline in cognitive abilities, including difficulties with problem-solving, decision-making, concentration, or learning new information.
- Everyday Tasks: Challenges in performing routine activities that were once familiar and easily accomplished, such as difficulty managing finances, following recipes, or completing household chores.
- Behavior: Unusual or uncharacteristic behaviors, such as increased confusion, agitation, aggression, or restlessness that cause concern or disruption in daily life.
- Personality: Noticeable changes in personality traits or emotional well-being, including shifts in mood, irritability, apathy, withdrawal from social activities, or loss of interest in hobbies.
It’s important to remember that experiencing one or more of these changes does not necessarily indicate dementia, as various factors can contribute to similar symptoms.
However, discussing your concerns with a healthcare professional will help determine the underlying cause and provide appropriate guidance and support.
How Dementia Impacts the Brain and Body

As dementia progresses, the brain deteriorates, leading to memory loss and impaired cognitive function. Basic bodily functions like breathing, digestion, and mobility are affected.
Eventually, individuals with advanced dementia require full-time assistance for essential tasks such as eating, walking, and communicating. They become susceptible to infections and may experience complications like pneumonia.
At this stage, many families opt for hospice care to prioritize comfort and quality of life.
Life Expectancy in Dementia
The life expectancy of a person with dementia can vary significantly depending on several factors.
On average, individuals with dementia live for about 8 to 10 years after the initial symptoms appear. However some individuals may live much longer or shorter lives.
It’s also worth mentioning that dementia is a progressive condition, meaning it worsens over time.
As the disease advances, individuals may experience increased cognitive decline, functional impairment, and other health complications. Quality of life and overall well-being become important considerations in the later stages of dementia.
Ultimately, it’s best to consult with healthcare professionals who can provide personalized information and guidance based on an individual’s specific situation and type of dementia.
Important Facts about Dementia

- Global Impact: Currently, more than 55 million people worldwide have dementia, with over 60% residing in low- and middle-income countries. Each year, nearly 10 million new cases are reported.
- Causes and Types: Dementia can be caused by various diseases and brain injuries. The most common form is Alzheimer’s disease, accounting for 60-70% of cases.
- Leading Cause: Dementia ranks as the seventh leading cause of death globally and is a major contributor to disability and dependence among older individuals.
- Economic Burden: In 2019, dementia cost economies around the world a staggering 1.3 trillion US dollars. Approximately 50% of these costs are attributed to informal caregivers, such as family members and close friends, who provide an average of 5 hours of daily care and supervision.
- Gender Disparity: Women are disproportionately affected by dementia, both directly and indirectly. They experience higher levels of disability-adjusted life years and mortality related to dementia. Additionally, women contribute to 70% of the caregiving hours for individuals living with dementia.