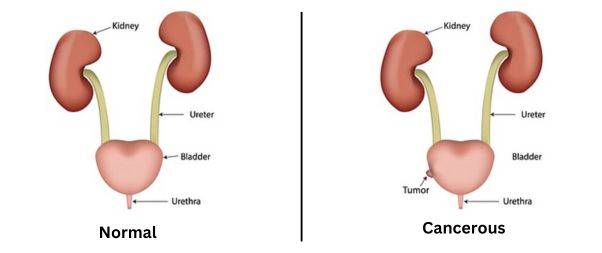
The bladder, a hollow muscular organ located in the lower abdomen, is responsible for storing urine. Bladder cancer starts in the cells of the bladder. It is characterized by the uncontrolled growth and division of abnormal cells in the lining of the bladder.
Early-stage bladder cancers are often detected, allowing for effective treatment. However, even after successful treatment, recurrence is possible, even in early-stage cases.
Consequently, individuals diagnosed with bladder cancer typically require regular follow-up tests for several years following treatment to monitor for any signs of recurrent bladder cancer.
Why does bladder cancer happen?
 The development of this cancer is often attributed to prolonged exposure to harmful substances that result in abnormal changes in the bladder cells over time.
The development of this cancer is often attributed to prolonged exposure to harmful substances that result in abnormal changes in the bladder cells over time.
One of the primary causes of bladder cancer is tobacco smoke. It is estimated that approximately half of all cases of bladder cancer are directly linked to smoking.
Additionally, contact with specific chemicals that were previously utilized in manufacturing processes is known to be a cause of bladder cancer. However, it is important to note that these substances have been banned since their harmful effects were recognized.
7 Signs of Bladder Cancer

Hematuria, the presence of blood or blood clots in the urine, is a common sign of bladder cancer. It is essential to consult a doctor if you notice blood in your urine, even if it appears cola-colored or if non-cancerous conditions can also cause hematuria.
Frequent urges to urinate with minimal urine output, often mistaken for a UTI, could potentially indicate bladder cancer, especially if you are over the age of 55.
Pain or a burning sensation during urination (dysuria) can be a symptom of various conditions, including bladder cancer. However, some bladder cancer patients may have blood in their urine without experiencing pain or burning during urination.
Pelvic or lower back pain can be a symptom of other common conditions, but it may indicate advanced bladder cancer if the cancer has spread to other parts of the body. If you have this symptom along with other signs of bladder cancer, prompt medical consultation is crucial.
Recurrent UTIs can be mistaken for bladder cancer. If you have received treatment for a UTI, but the symptoms persist, consider the possibility of bladder cancer.
Persistent fatigue that doesn’t improve with rest can be a symptom of advancing bladder cancer. If you consistently feel weak and lack energy for daily activities, seek medical attention.
Loss of appetite and unintentional weight loss are common side effects of bladder cancer and other cancers. While these symptoms can indicate other conditions, it is important to consult a healthcare professional for proper evaluation and diagnosis.
Risk Factors
Certain factors can increase the risk of developing bladder cancer. Here are the key risk factors:
Smoking: Smoking tobacco, including cigarettes, cigars, or pipes, is a significant risk factor for bladder cancer. Harmful chemicals in tobacco smoke can accumulate in the urine and damage the bladder lining, increasing the risk of cancer.
Increasing Age: Bladder cancer risk tends to rise with age. While it can occur at any age, the majority of people diagnosed with bladder cancer are over the age of 55.
Gender: Men are more likely to develop bladder cancer than women.
Exposure to Certain Chemicals: Occupational exposure to certain chemicals has been linked to an increased risk of bladder cancer. Chemicals such as arsenic and those used in dye, rubber, leather, textile, and paint manufacturing have been associated with bladder cancer risk.
Previous Cancer Treatment: Treatment with the anti-cancer drug cyclophosphamide and radiation therapy to the pelvic area for previous cancers can elevate the risk of bladder cancer.
Chronic Bladder Inflammation: Chronic or recurrent urinary infections or inflammations, such as those occurring with long-term use of a urinary catheter, may increase the risk of squamous cell bladder cancer. In certain regions, squamous cell carcinoma is associated with chronic bladder inflammation caused by a parasitic infection called schistosomiasis.
Personal or Family History of Cancer: Individuals who have previously had bladder cancer have a higher likelihood of developing it again. While bladder cancer is not commonly inherited, a family history of Lynch syndrome (hereditary nonpolyposis colorectal cancer) can increase the risk of bladder cancer, as well as cancers in the colon, uterus, ovaries, and other organs.
It’s important to note that having one or more risk factors does not necessarily mean a person will develop bladder cancer.
Conversely, some individuals without known risk factors may still develop the disease. Regular check-ups and discussing individual risk factors with a healthcare professional can help in understanding and managing the risk of bladder cancer.
Types
Bladder cancer can be classified based on its spread within the body. Here are the types:
Non-Muscle-Invasive Bladder Cancer (NMIBC): This is the most common type, accounting for around 7 out of 10 cases. In NMIBC, cancerous cells are confined to the inner lining of the bladder. It has not spread to the deeper muscle layers or other parts of the body.
While NMIBC is generally not life-threatening, it requires appropriate treatment and close monitoring to prevent recurrence.
Muscle-Invasive Bladder Cancer (MIBC): In MIBC, cancerous cells have spread beyond the inner lining and invaded the muscle layer of the bladder. This type is less common but carries a higher risk of metastasis (spreading) to other organs or lymph nodes.
MIBC is considered more aggressive and has the potential to be life-threatening if left untreated or not managed effectively.
Locally Advanced or Metastatic Bladder Cancer: When bladder cancer has progressed and spread to distant sites in the body, such as lymph nodes, bones, liver, or lungs, it is referred to as locally advanced or metastatic bladder cancer.
At this stage, the cancer has typically spread beyond the bladder and may require systemic treatments such as chemotherapy, immunotherapy, or targeted therapy.
The classification of bladder cancer into these types is important for determining the most suitable treatment approaches and predicting the prognosis.
Proper diagnosis and staging by healthcare professionals play a crucial role in guiding treatment decisions and managing the condition effectively.
Diagnosing

Bladder cancer involves a series of tests and examinations. Here are the common tests used to diagnose bladder cancer:
Urine Test: Your doctor may conduct a quick test to check for the presence of blood in your urine. A urine sample might also be sent to a laboratory for further analysis.
Internal Examination: Your doctor may perform an internal examination by inserting a gloved finger into your rectum (for males) or vagina (for females) to assess any abnormalities or tumors that can be felt.
- Ultrasound Scan: An ultrasound scan uses sound waves to create images of the bladder, kidneys, ureter, and urethra. It helps detect signs of cancer in the bladder and any blockages in the urinary system.
Cystoscopy: This procedure involves inserting a thin tube with a camera (cystoscope) into the bladder to visualize its interior. Biopsies (tissue samples) of the bladder lining may be taken during the cystoscopy to examine for cancer cells.
CT Urogram: A CT urogram combines a CT scan with a contrast dye to examine the kidneys, bladder, and ureters. It provides detailed images and helps determine the stage and location of the cancer.
Blood Tests: Blood tests can assess general health, liver function, kidney function, and blood cell counts, which provide important information about overall health and potential effects of cancer.
MRI Scan: Magnetic resonance imaging (MRI) uses magnetic fields and radio waves to create detailed images of the body. It helps assess the extent of the cancer, including whether it has invaded the deeper layers of the bladder or spread to other parts of the body.
CT Scan: Computed tomography (CT) scan uses x-rays and computer technology to produce cross-sectional images of the body. It can provide information about the location, size, and potential spread of bladder cancer.
PET-CT Scan: A PET-CT scan combines a CT scan with a positron emission tomography (PET) scan. It uses a radioactive tracer to detect areas of increased metabolic activity in the body, helping to evaluate the size, stage, and response to treatment of bladder cancer.
Bone Scan: A bone scan is used to check for any abnormalities or metastasis of bladder cancer in the bones. It may be conducted if there are symptoms suggesting bone involvement.
These tests, conducted by GPs and specialists, play a crucial role in diagnosing bladder cancer, determining its stage, and guiding appropriate treatment decisions.
Treatment

Treating bladder cancer involves different approaches depending on the stage and risk factors associated with the cancer. Here are the common treatment options:
- In Non-muscle-Invasive Bladder Cancer (NMIBC) the cancer is limited to the inner lining of the bladder.
Treatment typically starts with a surgical procedure called transurethral resection of a bladder tumor (TURBT). This involves removing cancerous cells while preserving the rest of the bladder.
After TURBT, chemotherapy medication may be instilled directly into the bladder to reduce the risk of cancer recurrence.
In some cases, Bacillus Calmette-Guérin (BCG), a medication that stimulates the immune system, may be injected into the bladder to lower the risk of cancer returning.
- In Muscle-Invasive Bladder Cancer (MIBC) it invaded the muscle layer of the bladder, and more aggressive treatment is required.
A common approach is surgically removing the entire bladder in a procedure called a cystectomy. After bladder removal, alternative methods for urine collection are necessary.
These can include creating an opening in the abdomen for urine to pass into an external bag or constructing a new bladder using a segment of the bowel.
Cystectomy may be accompanied by other treatments, such as chemotherapy or radiation therapy, to target any remaining cancer cells.
- Radiation Therapy and Chemotherapy
In cases where bladder removal is not recommended or feasible, a combination of radiation therapy and chemotherapy may be used as primary treatment.
This approach is often employed for individuals who have MIBC or are unfit for surgery. Sometimes chemotherapy is administered prior to surgery or in conjunction with radiation therapy.
Following treatment for any type of bladder cancer, regular follow-up tests will be conducted to monitor for potential recurrence or signs of cancer. These tests are important for ongoing surveillance and ensuring timely intervention if needed.
It is crucial to consult with a healthcare professional who can evaluate the specific characteristics of bladder cancer and guide you towards the most appropriate treatment plan.
Coping with a Bladder Cancer Diagnosis

It can be emotionally challenging, and changes in your body may affect how you feel about yourself. Support is available to help you through this process.
Here are some coping strategies and support options:
Dealing with Your Feelings:
- Understand that it is normal to have various emotions after a cancer diagnosis. You might feel shocked, upset, numb, frightened, uncertain, confused, angry, resentful, or guilty. Different feelings may come and go, and it’s important to allow yourself time to process and accept your emotions.
- Gathering information about your type of cancer and treatment can help you feel more informed and empowered. Make a list of questions to ask your doctor and bring someone along to appointments for support and to help remember the information provided.
- Take things one step at a time and seek help when needed. It’s okay to ask for assistance and support from healthcare professionals, family, and friends.
- Engage in practical activities like making lists, keeping a calendar of appointments, setting goals, and planning enjoyable activities to help you cope and maintain a sense of control.
Talking to Others:
- Talking to your friends, relatives, and healthcare providers about your cancer can provide valuable support. However, not everyone may be ready to talk about it, so respect their boundaries and communicate your needs openly.
- Cancer support groups, helplines, and online forums, such as Cancer Chat, can connect you with people who have had similar experiences and provide additional support.
- Consider seeing a counselor or therapist who specializes in cancer-related issues to help you navigate the emotional challenges and provide guidance.
Addressing Physical Changes:
- Bladder cancer and its treatments can lead to physical changes in your body. Discuss any concerns or physical changes with your doctor or specialist nurse, as they can help you manage them effectively.
- Problems passing urine, changes in appearance (such as scarring or a stoma), fatigue, and the impact on relationships and sex life are common issues. Seek support and information from healthcare professionals who can guide you through these changes and provide resources to cope with them.
Practical Coping:
- Alongside emotional and physical aspects, it’s important to address practical matters. Financial concerns, work-related issues, childcare, and other practical aspects may need attention. Seek guidance from social workers, financial advisors, or professionals specializing in supporting individuals with cancer.
Remember that you don’t have to face these challenges alone. Reach out to healthcare professionals, support organizations, and your loved ones for assistance. They can provide the support and resources you need to navigate the journey of cancer and its treatment.
Take Care of Yourself!
Also Read