“Exercise your way to a regular period – get started today!”
What are Periods?
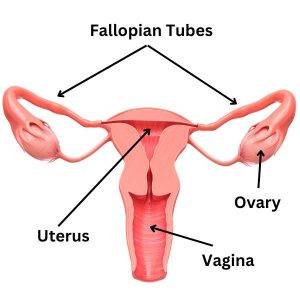
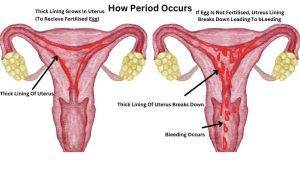
Periods, also known as menstrual periods or menstruation, are a normal and natural process that occurs in the female reproductive system. It is a monthly discharge of blood and other materials from the uterus, which typically lasts between 3 to 7 days.
Menstruation happens as a part of the menstrual cycle, which is the process of preparing the body for pregnancy each month.
The menstrual cycle is controlled by a complex interaction between hormones released by the brain and the ovaries.
If pregnancy does not occur during a menstrual cycle, the lining of the uterus that has built up in preparation for pregnancy is shed, resulting in the bleeding that occurs during a period.
Periods usually begin during puberty, which is when a girl’s body starts to change and develop, and continue until menopause, which is when a woman’s menstrual cycle stops.
The length and flow of periods can vary from person to person and may also be affected by factors such as age, weight, and overall health.
What Is Menstrual Pause?
The term “menstrual pause” is not commonly used in medical or scientific literature. However, it may refer to the cessation of menstruation that occurs during menopause.
Menopause is a natural biological process that marks the end of a woman’s reproductive years. It is defined as the permanent cessation of menstruation, which is confirmed after 12 consecutive months without a menstrual period. Menopause typically occurs between the ages of 45 and 55 but can occur earlier or later.
During menopause, the body’s production of estrogen and progesterone hormones decreases, which can cause a variety of symptoms such as hot flashes, night sweats, mood changes, and vaginal dryness.
Maintaining good health habits, such as regular exercise, a balanced diet, and consistent medical check-ups, is crucial for women experiencing menopause. These practices can help manage symptoms and lower the risk of developing certain health conditions.
Difference between the menstrual cycle and menopause
The menstrual cycle and menopause are two different phases of a woman’s reproductive life.
The menstrual cycle is a regular, cyclic process that occurs in women of reproductive age (usually from puberty until menopause).
It involves the shedding of the uterine lining, which results in menstrual bleeding, and the release of an egg from the ovary, which can potentially be fertilized by sperm.
Menopause, on the other hand, is a natural biological process that marks the end of a woman’s reproductive life. It occurs when the ovaries stop producing eggs and there is a decrease in the production of hormones such as estrogen and progesterone.
Menopause is diagnosed after a woman has gone 12 consecutive months without a menstrual period.
The menstrual cycle and menopause are related in that they are both part of a woman’s reproductive life, but they are distinct phases.
The menstrual cycle is a regular process that occurs monthly in women of reproductive age, while menopause is a transition that occurs as a woman approaches the end of her reproductive life.
Cause Of Periods
The menstrual cycle, which leads to periods, is a complex physiological process that is regulated by several hormones and organs in a woman’s body. The main causes of periods are as follows:
Hormonal Changes: The menstrual cycle is triggered by hormonal changes in a woman’s body. The hypothalamus in the brain produces gonadotropin-releasing hormone (GnRH), which stimulates the pituitary gland to release follicle-stimulating hormone (FSH) and luteinizing hormone (LH). These hormones then stimulate the ovaries to produce estrogen and progesterone, which are responsible for the growth and shedding of the uterine lining.
Uterine Lining Shedding: During the menstrual cycle, the uterine lining thickens in preparation for a potential pregnancy. If the egg released by the ovaries is not fertilized, the lining is shed, resulting in menstrual bleeding.
Ovulation: Ovulation is the release of an egg from the ovary, which typically occurs around day 14 of a 28-day menstrual cycle. If the egg is not fertilized, the menstrual cycle continues, and the uterine lining is shed.
Age: The onset of menstruation (menarche) typically occurs between the ages of 8 and 15 and is influenced by genetic, nutritional, and environmental factors. Menstruation stops at menopause, which occurs on average around the age of 50.
There can be other factors that may cause variations or changes in menstrual cycles, including stress, weight fluctuations, medications, and medical conditions such as polycystic ovary syndrome (PCOS), thyroid disorders, and reproductive system abnormalities.
Cycle Of Periods Or Phases Of Periods

The menstrual cycle is the physiological process that leads to the shedding of the uterine lining and results in menstrual bleeding. The menstrual cycle can vary in length and regularity between women, but on average it is a 28-day cycle. The cycle is divided into four phases:
Menstrual phase: This phase marks the beginning of the menstrual cycle and lasts for 3 to 7 days. It is characterized by the shedding of the uterine lining and the resulting menstrual bleeding.
Follicular phase: This phase lasts from the end of the menstrual phase to ovulation (around day 14 in a 28-day cycle). During this phase, the hypothalamus releases GnRH, which stimulates the pituitary gland to release FSH and LH. These hormones stimulate the ovaries to produce estrogen, which causes the uterine lining to thicken.
Ovulatory phase: This phase occurs around day 14 of a 28-day cycle and is characterized by the release of an egg from the ovary. This is triggered by a surge in LH, which causes the follicle to rupture and release the egg.
Luteal phase: This phase begins after ovulation and lasts until the next menstrual phase. The empty follicle left after ovulation forms the corpus luteum, which produces progesterone. Progesterone prepares the uterine lining for the potential implantation of a fertilized egg. If the egg is not fertilized, the corpus luteum disintegrates, causing a drop in progesterone levels and leading to the shedding of the uterine lining.
The menstrual cycle is a complex process involving the interplay of hormones and organs in a woman’s body.
Types Of Periods
There are several types of periods that women may experience, including:
Regular periods: These are periods that occur approximately every 28 days and last for 3 to 7 days. They are considered normal and healthy for most women.
Irregular periods: These are periods that occur outside of the normal 28-day cycle or have varying lengths. Irregular periods can be caused by a variety of factors, including stress, weight fluctuations, medical conditions, and hormonal imbalances.
Heavy periods: These are periods that involve excessive bleeding, lasting longer than seven days, and/or requiring the use of multiple tampons or pads. Heavy periods can be caused by medical conditions such as fibroids, polyps, or endometriosis.
Painful periods: These are periods that cause significant pain, cramping, and discomfort. Painful periods can be caused by a variety of factors, including hormonal imbalances, endometriosis, and pelvic inflammatory disease.
Absent periods: These are periods that do not occur for several months or longer. Absent periods can be caused by pregnancy, breastfeeding, hormonal imbalances, and medical conditions such as polycystic ovary syndrome (PCOS).
Light periods: These are periods that involve minimal bleeding and may last only a day or two. Light periods can be caused by hormonal imbalances, stress, and medical conditions such as thyroid disorders.
Women need to monitor their menstrual cycles and note any changes or irregularities. If a woman experiences significant changes in her periods, she should consult with her healthcare provider to determine the underlying cause and possible treatment options.
Are Periods Painful?
For many women, periods can be painful. The pain experienced during periods is commonly known as menstrual cramps or dysmenorrhea.
Menstrual cramps occur when the uterus contracts to help shed the lining, which causes pain and discomfort in the lower abdomen.
The severity of menstrual cramps can vary from woman to woman. Some women may experience mild cramping, while others may experience more intense pain that can interfere with their daily activities.
Other symptoms that can accompany menstrual cramps include headaches, fatigue, nausea, and diarrhea.
However, it’s important to note that not all women experience painful periods. Some women may have little to no discomfort during their periods.
Additionally, there are several treatment options available to help alleviate menstrual pain, such as over-the-counter pain medications, heat therapy, exercise, and relaxation techniques.
If you experience severe menstrual pain or other concerning symptoms during your period, it’s essential to consult with your healthcare provider to determine the underlying cause and possible treatment options.
How To Make Periods Less Painful?
There are several ways to make periods less painful. Some of these include:
Over-the-counter pain relievers: Over-the-counter pain relievers such as ibuprofen or naproxen can help alleviate menstrual cramps. Always follow the recommended dosage and check with your healthcare provider before taking any medication.
Heat therapy: Applying heat to the lower abdomen can help alleviate menstrual cramps. Use a heating pad or take a warm bath or shower to help relax the muscles and reduce pain.
Exercise: Gentle exercises such as walking, yoga, or stretching can help alleviate menstrual cramps. Exercise releases endorphins, which are natural pain relievers.
Dietary changes: Eating a balanced diet rich in fruits, vegetables, and whole grains can help alleviate menstrual pain. Avoiding caffeine, alcohol, and salty or processed foods may also help.
Herbal remedies: Some herbal remedies, such as ginger and chamomile tea, may help alleviate menstrual pain. Always check with your healthcare provider before using any herbal remedies.
Relaxation techniques: Practicing relaxation techniques such as deep breathing, meditation, or yoga can help reduce stress and alleviate menstrual pain.
Precaution needs to take during periods
There are several precautions that women can take during periods to manage menstrual discomfort and promote overall health and hygiene. Some of these precautions include:
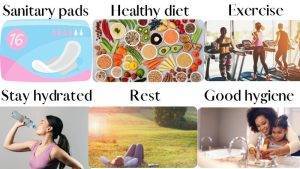
Use sanitary products: Use sanitary pads, tampons, or menstrual cups to manage menstrual bleeding. Change the pad or tampon every 4-6 hours, or as needed to maintain cleanliness.
Maintain good hygiene: Take a shower or bath at least once a day and change your sanitary pad or tampon regularly to prevent infections.
Eat a healthy diet: Eat a balanced diet with plenty of fruits, vegetables, and whole grains. Avoid caffeine, alcohol, and salty or processed foods, which can worsen menstrual symptoms.
Stay hydrated: Drink plenty of water and fluids to stay hydrated and help alleviate bloating and cramps.
Exercise: Regular exercise can help reduce menstrual cramps and improve overall mood and energy levels.
Rest: Get enough sleep and rest during your period to help alleviate fatigue and other menstrual symptoms.
Practice stress management: Stress can exacerbate menstrual symptoms, so it’s important to practice stress-reducing activities such as yoga, meditation, or deep breathing exercises.
It’s also important to seek medical attention if you experience severe menstrual pain, heavy bleeding, or other concerning symptoms during your period. Your healthcare provider can help diagnose and treat any underlying conditions that may be contributing to your menstrual discomfort.
Exercise To Help Make Periods Immediately
While exercise may not necessarily make periods come immediately, it can help regulate menstrual cycles and promote overall reproductive health.
Here are some exercises that may help regulate menstrual cycles:
Yoga: Practicing yoga can help reduce stress and promote relaxation, which can help regulate menstrual cycles. Some yoga poses, such as the seated forward bend and the child’s pose, may also help alleviate menstrual cramps.
Aerobic exercise: Aerobic exercises such as running, swimming, or cycling can help regulate menstrual cycles by reducing body fat and promoting overall reproductive health.
Strength training: Strength training exercises such as weightlifting or resistance training can help regulate menstrual cycles by promoting hormonal balance and reducing body fat.
While exercise can be beneficial in regulating menstrual cycles and promoting reproductive health, excessive exercise or over-exertion can have the opposite effect and disrupt menstrual cycles. Always consult with your healthcare provider before starting a new exercise regimen, especially if you have underlying health conditions or concerns about your menstrual cycles.
Things Helpful In Periods
Here are some things that can be helpful during periods:
A heating pad or hot water bottle: Applying heat to the lower abdomen can help alleviate menstrual cramps. Use a heating pad or hot water bottle to help relax the muscles and reduce pain.
Comfortable clothing: Wear comfortable, loose-fitting clothing during your period to reduce discomfort and allow for better circulation.
Proper hygiene: Good hygiene is important during periods to prevent infections. Change your sanitary pad or tampon regularly, wash your hands often, and take a shower or bath at least once a day.
Hydration: Drink plenty of water and fluids to stay hydrated and help alleviate bloating and cramps.
Healthy diet: Eating a balanced diet rich in fruits, vegetables, and whole grains can help alleviate menstrual pain. Avoiding caffeine, alcohol, and salty or processed foods may also help.
Rest: Get enough sleep and rest during your period to help alleviate fatigue and other menstrual symptoms.
Pain relievers: Over-the-counter pain relievers such as ibuprofen or naproxen can help alleviate menstrual cramps. Always follow the recommended dosage and check with your healthcare provider before taking any medication.
Support network: Having a support network of friends and family who understand and can provide emotional support during your period can be helpful.
Every woman’s experience with periods is different, so it’s essential to find what works best for you in terms of managing menstrual discomfort and promoting overall health and hygiene. If you experience severe menstrual pain or other concerning symptoms during your period, it’s essential to consult with your healthcare provider to determine the underlying cause and possible treatment options.