“Get Moving to Beat Varicose Veins – Exercise Your Way to Better Health!”
What are Varicose veins?
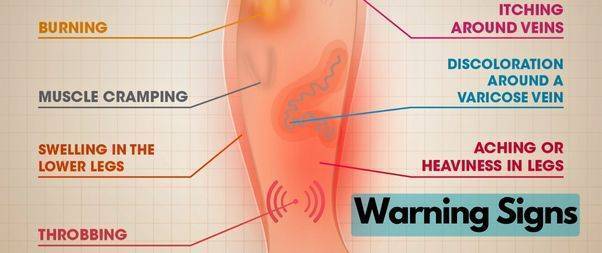
The enlarged, twisted, and swollen veins commonly appear on the legs and feet and can be painful and uncomfortable.
They may also be accompanied by other symptoms such as aching, heaviness, and swelling in the affected area. They may also cause skin discoloration, itching, and a feeling of fatigue or weakness in the legs.
Varicose veins are often more common in women than men.
Why does Varicose Vein Happen?
Veins are blood vessels that carry deoxygenated blood from the body back to the heart.
These veins happen when the valves inside the veins do not work properly, causing blood to flow backward and pool inside the veins.
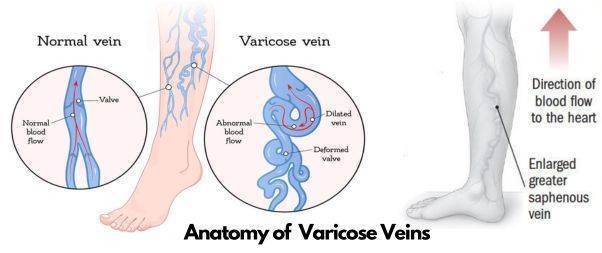 In healthy veins, the valves ensure that blood flows in one direction and does not flow backward. However, in varicose veins, the valves become weak or damaged, causing blood to pool inside the veins.
In healthy veins, the valves ensure that blood flows in one direction and does not flow backward. However, in varicose veins, the valves become weak or damaged, causing blood to pool inside the veins.
Normally, blood flows from the legs to the heart against the force of gravity. Valves in the veins help to keep the blood flowing in the right direction.
However, if the valves become weak or damaged, blood can pool in the veins, causing them to stretch and twist, leading to varicose veins.
Causes of Varicose Vein
Several factors are thought to contribute to the development, including:
Age: As we age, the valves in our veins can become weaker, making them more prone to leaking.
Genetics: Varicose veins tend to run in families, so if your parents or siblings have them, you may be more likely to develop them too.
Gender: Women are more likely to develop varicose veins than men, likely due to hormonal changes during pregnancy and menopause.
Prolonged sitting or standing: Being in one position for long periods can put extra pressure on your veins, which can contribute to their weakening.
Obesity: Carrying excess weight can put extra pressure on your veins, making them more likely to become damaged.
Injury: A previous injury to the leg, such as a fracture, can damage the veins and contribute to the development of varicose veins.
Medical conditions: Certain medical conditions, such as deep vein thrombosis (DVT) and phlebitis, can damage the valves in the veins and lead to the development of varicose veins.
Are There Different Types Of Varicose Vein?
Several types of varicose veins can affect different parts of the body. The most common type is found in the legs, but it can also occur in other areas such as the pelvis, uterus, and rectum.
Here are some of the different types of varicose veins:
Varicose veins in the legs: These are the most common type of varicose vein and can be seen as bulging, twisted veins just beneath the skin’s surface. They are often blue or purple and can be accompanied by symptoms such as pain, swelling, and heaviness in the legs.
Spider veins: These are small, thin veins that are usually red or blue and can be seen just beneath the skin’s surface. They are often found on the legs or face and are typically a cosmetic concern rather than a medical issue.
Pelvic varicose veins: These are varicose veins that occur in the pelvic area and can cause pain, discomfort, and pressure in the lower abdomen, hips, and thighs. They are more common in women and can be caused by pregnancy, hormonal imbalances, or other factors.
Vulvar varicose veins: These are varicose veins that occur in the vulva, which is the outer part of the female genitalia. They can cause pain and discomfort during sexual activity, and may also cause swelling and a feeling of pressure in the pelvic area.
Hemorrhoids: These are varicose veins that occur in the rectum and anus, and can cause pain, itching, and bleeding. They are more common in pregnant women and those with a family history of hemorrhoids.
It’s important to note that while varicose veins can cause discomfort and pain, they are usually not a serious medical condition and can often be managed with lifestyle changes or medical treatments. If you are experiencing symptoms of varicose veins, it’s a good idea to speak with your doctor to determine the best course of treatment for your situation.
Exercises To Prevent Varicose Vein
Exercise can be beneficial in managing the symptoms of varicose veins and improving blood circulation. Here are some exercises that can help:

Walking: Walking is a low-impact exercise that can help improve circulation and strengthen the muscles in the legs. It’s important to wear comfortable shoes and walk on a flat surface.
Cycling: Cycling is another low-impact exercise that can help improve circulation in the legs. It’s important to adjust the seat height to prevent putting too much pressure on the veins.
Swimming: Swimming is a great exercise that can help improve circulation and reduce swelling in the legs. It’s important to avoid strokes that require the legs to be held in a horizontal position for extended periods.
Leg lifts: Lie on your back and lift one leg at a time to a 45-degree angle. Hold for a few seconds and then lower your leg back down. Repeat with the other leg. This exercise helps to strengthen the muscles in the legs and improve circulation.
Calf raises: Stand with your feet hip-width apart and lift up onto your toes. Hold for a few seconds and then lower your heels back down. This exercise helps to strengthen the calf muscles and improve circulation in the legs.
It’s important to consult with a healthcare provider before starting any exercise program, especially if you have varicose veins. They can provide guidance on the types of exercises that are safe and effective for your individual needs.
Treatments

Some common treatments for varicose veins:
Lifestyle changes: Making changes to your lifestyle can help alleviate the symptoms of varicose veins. These changes include exercising regularly, losing weight, avoiding prolonged periods of standing or sitting, and elevating your legs.
Compression stockings: Compression stockings apply pressure to the legs and can help improve circulation, reducing the appearance and discomfort of varicose veins.
Sclerotherapy: Sclerotherapy is a minimally invasive procedure where a solution is injected directly into the affected veins, causing them to collapse and fade away over time.
Endovenous Laser Treatment (EVLT): EVLT is a minimally invasive procedure that uses a laser to close off the affected veins, causing them to shrink and eventually disappear.
Ambulatory phlebectomy: Ambulatory phlebectomy is a surgical procedure that involves making small incisions in the skin and removing the affected veins.
Endoscopic vein surgery: Endoscopic vein surgery is a more invasive surgical procedure that involves using a small camera to visualize and remove the affected veins.
Do not forget to consult with a healthcare provider to determine the best treatment option for your individual case.
Can Yoga help in preventing varicose veins?
Yes, practicing yoga regularly can help in preventing varicose veins. Yoga involves stretching and strengthening exercises that can improve circulation and reduce the risk of developing varicose veins.
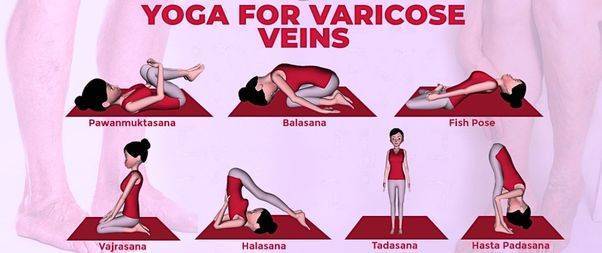
Here are some yoga poses that can be particularly beneficial:
Viparita Karani (Legs-Up-the-Wall Pose): This pose helps to reduce swelling and improve circulation in the legs.
Tadasana (Mountain Pose): This pose helps to improve posture and promote blood flow throughout the body.
Trikonasana (Triangle Pose): This pose helps to stretch and strengthen the legs, improving circulation and reducing the risk of varicose veins.
Ardha Matsyendrasana (Half Lord of the Fishes Pose): This pose helps to improve digestion and promote blood flow to the abdominal region.
Balasana (Child’s Pose): This pose helps to reduce stress and tension in the body, which can help to improve circulation and reduce the risk of varicose veins.
In addition to these poses, regular yoga practice can help to improve overall fitness, reduce stress, and promote a healthy lifestyle, which can all contribute to preventing varicose veins. However, if you already have varicose veins, it’s important to consult with a healthcare provider to determine the best course of treatment.
How to Avoid Injury When Exercising with Varicose Veins
 Exercising with varicose veins can be a challenge, but it doesn’t have to be.
Exercising with varicose veins can be a challenge, but it doesn’t have to be.
Here are some tips to help you exercise safely with varicose veins:
1. Start slow. When beginning a new exercise routine, it’s important to start slow and gradually increase the intensity. This will help your body adjust to the new activity and reduce the risk of injury.
2. Wear compression stockings. Compression stockings can help reduce swelling and discomfort in the legs. They also help improve circulation, which can help reduce the risk of injury.
3. Choose low-impact activities. High-impact activities like running and jumping can put extra strain on your veins and increase the risk of injury. Instead, opt for low-impact activities like swimming, walking, and cycling.
4. Take breaks. If you start to feel pain or discomfort, take a break and rest. This will give your veins time to recover and reduce the risk of injury.
5. Stretch. Stretching before and after exercise can help reduce the risk of injury. It can also help improve circulation and reduce swelling in the legs.
By following these tips, you can stay active and healthy while avoiding injury. With the right precautions, you can exercise safely with varicose veins.