In this Page
When your child is diagnosed with Spinal Muscular Atrophy (SMA), it can feel overwhelming.
The path ahead may seem uncertain, but there’s a whole community here for you – doctors, therapists, and families just like yours who are navigating this journey too.
SMA is a genetic condition that primarily affects the motor neurons in the spinal cord, leading to muscle weakness and mobility issues. Over time, some children may develop additional complications.
Remember, every child’s journey with SMA is unique. And though there will be challenges, there will also be moments of joy, triumph, and immense pride.
This journey may be unexpected. Your strength, combined with the support of the community and healthcare providers, will guide you and your child through the journey of SMA .
What is SMA?
 Spinal Muscular Atrophy (SMA) is a genetic disorder characterized by weakness and wasting (atrophy) in muscles used for movement (skeletal muscles).
Spinal Muscular Atrophy (SMA) is a genetic disorder characterized by weakness and wasting (atrophy) in muscles used for movement (skeletal muscles).
It is caused by a loss of specialized nerve cells, called motor neurons, in the spinal cord and the part of the brain that is connected to the spinal cord (the brainstem). This loss leads to physical disability.
Types of SMA
SMA is characterized by multiple types, each with varying degrees of severity and onset ages. All types result in muscle weakness and movement difficulties, though the severity varies.
However, none of the types affect cognitive capabilities or learning potential.
Type 1 SMA, also known as Werdnig-Hoffman disease, affects infants within the first 6 months. These infants:
- Experience extreme muscle weakness and floppiness (hypotonia)
- Struggle with movement, eating, breathing, and swallowing
- Cannot lift their head or sit without assistance
Type 2 SMA appears in older infants and toddlers, typically between 7 to 18 months. Its symptoms are less severe than Type 1. Children with this condition:
- Can possibly sit unaided but can’t stand or walk
- Exhibit weak arms or legs
- Experience trembling in fingers and hands
- May develop joint issues, like abnormal spinal curvature (scoliosis)
- May have weak breathing muscles and difficulty coughing, leading to potential chest infection risks
- Life expectancy varies, and some individuals live into adolescence or adulthood.
Type 3 SMA, also known as Kugelberg-Welander disease, affects children and young adults, with symptoms typically manifesting after 18 months.
Onset can be highly variable, sometimes not appearing until late childhood or early adulthood. People with this type:
- Can stand and walk independently, though they may struggle with walking or rising from a sitting position
- Might have balance issues, running or climbing steps difficulty, and slight finger trembling
- May find walking increasingly challenging over time, possibly losing the ability to walk as they age For more on
Type 4 SMA, or adult-onset SMA, generally begins in early adulthood. Individuals with this condition may exhibit:
- Weakness in hands and feet
- Difficulty walking
- Shaking and muscle twitching Type 4 SMA gradually worsens over time but typically doesn’t affect breathing or swallowing.
- This type is generally less severe, and individuals have a normal life expectancy.
There are also other SMA variants, including:
- Spinal Muscular Atrophy with Respiratory Distress (SMARD): Diagnosed in a baby’s first year and can cause significant breathing problems.
- Kennedy’s Disease or Spinobulbar Muscular Atrophy (SBMA): A rare SMA type that only affects men and usually begins in middle age; typically doesn’t affect life expectancy.
- Distal Spinal Muscular Atrophy (DSMA): Affects mainly the hands, feet, lower arms, and lower legs.
How SMA is Caused

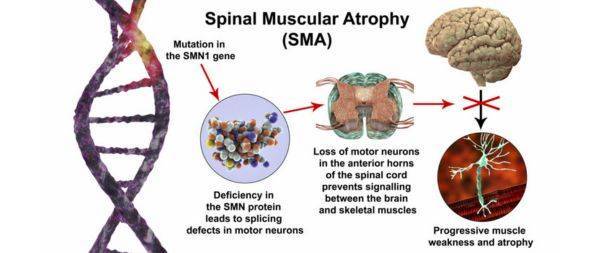
SMA is caused by mutations in the SMN1 gene. This gene provides instructions for making a protein called Survival Motor Neuron (SMN), which is critical for the maintenance of motor neurons.
If the SMN1 gene is mutated, the body cannot produce enough SMN protein, leading to the degeneration of motor neurons and resulting in muscle weakness.
How SMA is Inherited
SMA is typically an inherited condition, meaning it’s passed down from parents to their children via genes.
In most situations, a child is at risk of being born with SMA if both parents carry a defective gene linked to the disease.
These parents usually do not have SMA themselves, making them what we call “carriers”. It is estimated that around 1 in 40 to 60 people are carriers of the primary gene mutation causing SMA.
When both parents are carriers, the probabilities for their offspring are as follows:
- There’s a 25% (or 1 in 4) chance that their child will inherit SMA.
- There’s a 50% (or 1 in 2) chance that their child will become a carrier of the defective gene but will not develop SMA.
- There’s a 25% (or 1 in 4) chance that their child will neither inherit SMA nor be a carrier.
It’s worth noting that some of the less common types of SMA may be inherited differently, or might not be inherited at all.
If you or your partner have a family history of SMA and are concerned about the risk to your children, it’s recommended to consult a healthcare provider.
Warning Signs

The manifestation and initial onset of SMA symptoms largely depend on the specific type of SMA one has.
Common symptoms encompass:
- Limbs that are weak or exhibit a floppy nature
- Challenges with movement, for instance, difficulties in sitting up, crawling, or walking
- Muscle tremors or shaking
- Bone and joint complications, like an abnormal curvature of the spine, also known as scoliosis
- Issues with swallowing
- Breathing complications
It’s important to note that SMA does not influence intellectual abilities or result in learning disabilities.
Diagnosis
There are a variety of assessments that can determine whether you or your child has SMA, or whether you’re at risk of conceiving a child with the condition.
Pre-pregnancy Testing
If you’re considering having a baby and you’ve previously had a child with SMA, or there’s a history of SMA in your family or your partner’s family, you should consult your primary care physician.
Your doctor may suggest genetic counseling to help you comprehend the possibility of your child developing SMA.
A genetic test can be conducted to establish if you carry the gene mutation associated with the disease.
If you’re potentially at risk of having a child with SMA, discussing your options with your genetic counsellor is advisable. These options may include:
- Proceeding with pregnancy and either waiting to see if your child is born with SMA, or conducting prenatal tests to determine if they will have the condition.
- Using donor sperm or eggs for conception.
- Opting for pre-implantation genetic diagnosis (PGD) – a procedure where fertilization occurs in a laboratory, the resultant embryos are tested for SMA, and only unaffected embryos are transferred to the womb.
Prenatal Testing
If you’re pregnant and there’s a risk your child may have SMA, there are tests available to check for the condition. The primary tests are:
- Chorionic Villus Sampling (CVS) – a procedure where placental cells are tested, usually between the 11th to 14th weeks of pregnancy.
- Amniocentesis – a procedure where amniotic fluid is tested, typically between the 15th to 20th weeks of pregnancy.
Both these tests carry a slight risk of miscarriage. If the tests indicate that your baby is likely to have SMA, you should discuss the implications and your options with your doctor.
Post-birth Testing
If you or your child display symptoms typical of SMA, a genetic blood test can be performed to confirm the diagnosis.
You may also be queried about any family history of conditions affecting nerves and muscles. A physical examination may be conducted to check for signs of SMA or related conditions.
On rare occasions, additional tests may be required. For instance:
- Electromyography – a procedure involving the insertion of thin needles into a muscle to evaluate its functionality.
- Muscle Biopsy – a procedure where a small muscle sample is extracted for examination.
Treatment

While there is currently no known cure for SMA, ongoing research is aimed at discovering new treatment options.
Existing treatment and support measures are designed to manage symptoms and help individuals with the condition maintain the best possible quality of life.
Your care or your child’s care will be facilitated by a team of healthcare professionals, who will work together to formulate a comprehensive care plan outlining the necessary support and treatment approaches.
Nutrition and Dietary Support
Ensuring appropriate nutrition is particularly important for individuals with SMA, especially children, to promote healthy growth and development. Dietary guidance can be provided by a dietitian.
If feeding or swallowing poses challenges, the use of a feeding tube might be necessary. This could be a tube directly attached to the stomach through the skin (gastrostomy tube), or a tube inserted through the nose and down the throat (nasogastric tube).
Respiratory Support
Various treatments are available to address the breathing difficulties that can occur in individuals with SMA. These may include:
- Breathing exercises to fortify breathing muscles and facilitate coughing.
- A suction machine to clear the throat, if necessary. This involves a thin plastic tube that is inserted into the back of the throat to suction away mucus.
- In more severe cases, a device that supplies air via a mask or tube.
You may also be advised to get vaccinations against flu and pneumonia to reduce your risk of severe illness from these infections.
Mobility and Assistive Equipment

If movement is challenging for you or your child, advice and support can be provided by an occupational therapist or physiotherapist. They can provide guidance on:
- Mobility aids such as walking frames and wheelchairs
- Supports for the limbs (splints or braces)
- Shoe inserts to assist walking (orthotics)
Physical Therapy
Exercises and stretches can help maintain strength and prevent joint stiffness. A physiotherapist can recommend suitable exercises.
The extent of exercise you or your child can perform will depend on the severity of your condition, but it’s beneficial to remain as active as possible.
Treatment for Spinal Complications
Some children with SMA may develop an abnormally curved spine, known as scoliosis. Treatments include:
- A custom-made back brace to provide support and guide the spine’s correct growth.
- Spinal surgery to straighten the spine with metal hooks and rods, followed by a bone fusion procedure.
Medication

Several medications are used to treat certain types of SMA, including:
- Nusinersen (Spinraza) – a medicine that targets the defective gene, administered as a spinal injection every few months.
- Risdiplam (Evrysdi) – a medicine that targets the backup copy of the defective gene, administered as a daily oral liquid.
- Onasemnogene abeparvovec (Zolgensma) – a gene therapy that delivers a healthy copy of the gene causing the condition, administered as a single injection.
Your treatment team will advise whether these medicines are appropriate for you or your child, depending on the type of SMA, age, and symptoms.
These highly powerful medications also have some side effects mostly on the liver. So steroids are prescribed by the doctors.
These treatments have shown promise, especially when given early in the course of the disease.
New Treatment Research
Research into potential new treatments for SMA is ongoing. You can ask your medical team about current clinical trials exploring new treatments or check the SMA clinical trials database to stay informed about ongoing research.
Ishani- A Warrior of SMA Type 2

Ishani, a 3+year-old survivor of Spinal Muscular Atrophy-type 2 living in Meerut, Uttar Pradesh India.
Born on 27 August 2019, Ishani was diagnosed with SMA type 2 when she was 8 months old, she had started showing symptoms of SMA like usual patients when she was 7 months old.
SMA, a disease never heard in the Verma family and was unfamiliar to all, they couldn’t have imagined Ishani would be a part of the 1 out of 10,000 SMA patients in India. There was no family history of it from both of the parent’s sides and they hence lacked the knowledge of it.
The initial days involved waves of worry. Physical, financial, and mental struggle in the whole Verma family. There were times when they had no clue which path to go on!
Fortunately, the family managed to get the most expensive requisite drug Zolgensma by Novartis for Ishani. She is the first girl of SMA Type-2 who got her medicine in AIIMS on 17th June 2020.
However, their hope of seeing Ishani walk on her own after getting the drug crashed soon. The journey of struggle is still not over, the drug doesn’t prevent the risk of other diseases. She is still not able to even stand on her own. She has to wear braces and special shoes to stand due to Scoliosis and backbone issues.
Scans and checkups for her backbone, bone marrow, physiotherapy sessions, and vital medications prescribed by professional doctors are still in progress.
Ishani needs special attention from her parents due to SMA but she has some extraordinary qualities developed in her like her brain is so sharp and she is so intelligent more than a normal child.
I pray for her wellness to recover soon.
All the Best Ishani!