Highlights
Richard Ramirez, also known as “The Night Stalker,” is a well-known name in the annals of American criminal history.
Born Ricardo Leyva Muñoz Ramirez on February 29, 1960, he was notorious for his crime spree in Los Angeles and San Francisco between 1984 and 1985.
His infamous activities culminated in multiple counts of murder, rape, burglary, and sodomy, which made headlines nationwide and triggered widespread fear.
But besides his criminal history, there is another aspect of his life that has garnered attention – his battle with cancer.
Ramirez’s Disease
In the years following his conviction and subsequent imprisonment, Ramirez’s health began to deteriorate.
In 2013, the infamous serial killer was diagnosed with B-cell lymphoma, a type of cancer that begins in the B-cells – a type of white blood cell that plays a crucial role in fighting infections by producing antibodies.
What is B-Cell Lymphoma?
 B-cell lymphoma is a type of cancer that primarily affects the B-cells, a type of white blood cell that’s integral to the immune system.
B-cell lymphoma is a type of cancer that primarily affects the B-cells, a type of white blood cell that’s integral to the immune system.
B-cells are responsible for producing antibodies to combat infections, making them a crucial part of our body’s defense mechanism.
The term “B-cell lymphoma” actually refers to a group of cancers, as there are several different types that can develop in different kinds of B-cells.
These lymphomas can be broadly categorized into two types:
- Hodgkin’s lymphomas
- Non-Hodgkin’s lymphomas
with the latter being more common.
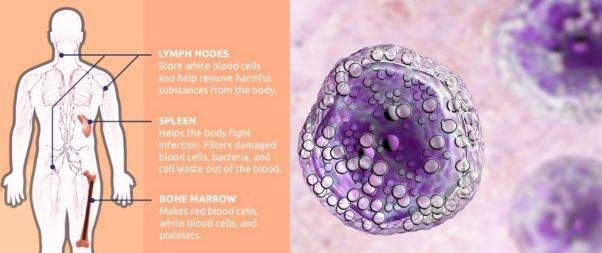
B-cell lymphomas can develop in various parts of the body, including the
- Lymph nodes
- Spleen
- Bone marrow
- Blood
- Other organs where lymph tissue is found.
Types of B-Cell Lymphoma
When your doctor diagnosis you with B-cell lymphoma, they’ll let you know exactly what kind you have.
The most common kind of non-Hodgkin’s lymphoma is known as Diffuse large B-cell lymphoma (DLBCL).
There are also other kinds of B-cell non-Hodgkin’s lymphoma, including:
Follicular lymphoma: This type grows slowly and usually affects older people.
Chronic lymphocytic leukemia/small lymphocytic leukemia (CLL/SLL): These are closely related types that grow slowly.
Mantle cell lymphoma: This type grows quickly.
Marginal zone lymphoma: This kind features small cells and grows slowly.
Burkitt lymphoma: This is a rare disease that grows very fast.
Lymphoplasmacytic lymphoma (Waldenstrom macroglobulinemia): This is a rare type that grows slowly.
Primary mediastinal large B-cell lymphoma: This is a rare type that mostly affects young adults and is more common in women.
Warning Signs
 The symptoms of B-cell lymphoma can vary widely based on the specific type and the stage of the disease.
The symptoms of B-cell lymphoma can vary widely based on the specific type and the stage of the disease.
However, some common signs and symptoms often associated with this group of cancers include:
Swollen lymph nodes: Often noticed in the neck, armpit, or groin, these are usually painless and one of the first signs of lymphoma. However, swollen lymph nodes can also result from infections and are not exclusively indicative of lymphoma.
Fever: Persistent or recurrent fevers can occur as the body responds to cancerous cells.
Night sweats: These can be severe enough to soak clothing and bedding.
Unexplained weight loss: Significant, unintentional weight loss could be a sign of many types of cancer, including lymphoma.
Fatigue: This could be a result of the body’s energy being redirected to fighting the cancerous cells, or it could be due to the cancer cells affecting the body’s normal metabolic processes.
Coughing or shortness of breath: This can occur if the lymphoma affects lymph nodes in the chest, causing them to press on the windpipe (trachea).
Pain or bloating in the abdomen: This can occur if the lymphoma affects lymph nodes in the abdomen or if the disease enlarges the spleen.
Loss of appetite: People with lymphoma sometimes feel full after only a small amount of food, leading to a loss of appetite.
Itchy skin or rash: This could be a symptom of lymphoma, although there are many other more common causes of these symptoms.
These symptoms can also be caused by many other conditions, most of which are far less serious than cancer.
However, anyone experiencing persistent or unexplained symptoms should consult with a healthcare provider to ensure an accurate diagnosis and appropriate treatment.
Causes and Risk factors
It appears to develop from genetic mutations in the B-cells. These mutations cause the B-cells to grow and divide out of control, forming a tumor.
The abnormal cells can also continue to live when normal cells would die. Over time, these abnormal B-cells accumulate and form a tumor, leading to lymphoma.
Certain factors can increase the risk of developing B-cell lymphoma:
Age: The risk of B-cell lymphoma increases with age.
Compromised Immune System: Those with weakened immune systems, such as people living with HIV/AIDS or those who take immune-suppressing medications (like those used following organ transplants), are more susceptible.
Autoimmune Diseases: Conditions that cause the immune system to attack the body’s own cells, such as rheumatoid arthritis or lupus, can increase the risk of B-cell lymphoma.
Exposure to Certain Chemicals: Certain chemicals, particularly those associated with specific industries like farming, can increase the risk. For example, exposure to pesticides or solvents has been linked to an increased risk of lymphomas.
Infections: Certain viral and bacterial infections can increase the risk of specific types of non-Hodgkin’s lymphoma. Examples include the Epstein-Barr virus, which causes mononucleosis, the human T-cell leukemia/lymphoma virus (HTLV-1), Hepatitis C, and the bacterium Helicobacter pylori.
Family History: Having a close relative who has had lymphoma can slightly increase the risk of the disease.
However, many people with these risk factors never develop lymphoma, and many who do get the disease have none of these risk factors.
As with many types of cancer, the development of B-cell lymphoma likely involves a complex interaction of genetic, environmental, and lifestyle factors.
Diagnosis

Diagnosing B-cell lymphoma usually involves a series of steps to help confirm the presence of cancer cells, identify the type of lymphoma, and determine how far it’s spread (the stage).
Here’s a simplified process of how B-cell lymphoma is typically diagnosed:
Medical History and Physical Examination: The process begins with a thorough review of the patient’s medical history and a physical exam. The doctor will ask about symptoms, lifestyle, past health issues, and family history of diseases. They will also check for physical signs of lymphoma such as swollen lymph nodes in the neck, underarms, or groin, as well as swelling or pain in the abdomen.
Blood Tests: Blood tests can provide information about the overall health and how well the organs are functioning. They can also sometimes show signs of lymphoma.
Biopsy: A biopsy is usually needed to definitively diagnose lymphoma. This involves taking a small sample of tissue from an enlarged lymph node or other affected area, which is then examined under a microscope by a pathologist. The pathologist looks for cancerous cells and can identify the specific type of lymphoma.
Bone Marrow Examination: This test may be done to see if the lymphoma has spread to the bone marrow. A small sample of bone marrow is removed, usually from the hip bone, using a long, fine needle, and then examined under a microscope.
Imaging Tests: Tests such as CT, PET, or MRI scans can help to determine the spread of the disease throughout the body. This helps in “staging” the disease, which in turn helps determine the best treatment options.
Lumbar Puncture (Spinal Tap): This might be done if there’s a concern that the lymphoma has spread to the spinal fluid. A small sample of cerebrospinal fluid (CSF) is removed from the spinal canal and checked for lymphoma cells.

Experiencing potential symptoms of lymphoma to seek medical advice as early as possible, as early detection can significantly improve the prognosis and treatment outcomes.
Treatment
The treatment for B-cell lymphoma can vary widely depending on the type of lymphoma, its stage, the patient’s overall health, and the patient’s personal preferences.
Here are some commonly used treatment options for B-cell lymphoma:
Chemotherapy: This is often the first line of treatment for many types of lymphoma. It involves using drugs to kill cancer cells. These drugs can be given intravenously or orally and work by interrupting the cell division process of the cancer cells.
Radiation therapy: This treatment uses high-energy beams, like X-rays or protons, to kill cancer cells. It’s often used for treating early-stage lymphomas or as a palliative treatment to relieve symptoms in advanced stages of the disease.
Immunotherapy: This treatment harnesses the power of the patient’s immune system to fight cancer. Drugs like rituximab (Rituxan) are used in some B-cell lymphomas to enhance the body’s natural defenses against the cancer.
Targeted therapy: These are drugs that specifically target the vulnerabilities of the cancer cells. For example, ibrutinib (Imbruvica) and idelalisib (Zydelig) block a specific protein that B-cell lymphomas need to survive and grow.
CAR-T cell therapy: This is a relatively new type of treatment where a patient’s T-cells (a type of immune system cell) are genetically engineered to produce receptors on their surface called chimeric antigen receptors (CARs). These receptors can recognize and kill the cancer cells. This therapy is usually considered for patients whose cancer has not responded to other treatments.
Stem cell transplant: This procedure allows doctors to use higher doses of chemotherapy than usual. After chemotherapy, the patient receives a transplant of stem cells to help rebuild their bone marrow.
Radioimmunotherapy: This treatment combines a radioactive particle with an antibody that targets the cancer cells. The antibody delivers the radiation directly to the cancer cells, limiting the damage to healthy cells.
Each of these treatments has potential side effects, and the best approach often involves a combination of different treatments.
Living With
Living with B-cell lymphoma can present several challenges, as it requires not only dealing with the physical effects of the disease and its treatments but also managing the emotional and psychological impacts.
Here are some aspects to consider when living with B-cell lymphoma:
Managing Symptoms and Side Effects: Both the disease itself and its treatments can cause various symptoms and side effects, such as fatigue, pain, nausea, and weight changes. It’s essential to communicate these issues with your healthcare team, as they can suggest ways to manage them.
Maintaining Nutrition: Proper nutrition can help you feel better, maintain strength, and cope with the side effects of treatment. A dietitian can help create a dietary plan that meets your specific needs.
Staying Active: While it’s important to rest and take care of your body, maintaining a level of physical activity can improve your mood, help manage side effects like fatigue, and generally promote better health.
Psychological and Emotional Support: It’s normal to experience a range of emotions when living with lymphoma, including anxiety and depression. Speaking with a therapist or counselor, joining a support group, or confiding in close friends or family can help manage these feelings.
Regular Monitoring and Follow-up: Regular check-ups are critical to monitor the progress of the disease, assess how well the body is responding to treatment, and make adjustments as necessary.
Financial Considerations: The cost of cancer treatment can be a significant concern. Social workers or financial advisors familiar with healthcare situations can help explore what financial assistance, insurance coverage, or funding options may be available.
Communication: Keep an open line of communication with your healthcare team. Don’t hesitate to ask questions about anything you don’t understand or worry about.
Ramirez’s Survival
Richard Ramirez passed away on June 7, 2013, at Marin General Hospital in Greenbrae, California, less than three months after his cancer diagnosis.
He was 53 years old. Given Ramirez’s imprisonment, he likely had limited personal support and faced additional challenges managing his health condition.
His journey was undoubtedly marked by the physical discomfort and emotional strain typical of cancer, but it was also uniquely framed by his status as a death row inmate.
While it is difficult to determine how long he may have been living with the disease before it was diagnosed, his case illustrates the often aggressive nature of B-cell lymphomas and the importance of early detection and treatment.
In a Nutshell
Ramirez’s experience with B-cell lymphoma underscores that cancer can affect anyone, regardless of their circumstances.
His journey with the disease, however, was marked by unique challenges given his status as a prisoner, limiting his access to support and potentially impacting his overall care and treatment experience.