Cervical Intraepithelial Neoplasia grade 3 (CIN3), an often alarming diagnosis, refers to significant abnormal changes within the cervical cells.
It’s deemed a pre-cancerous state that carries the risk of developing into invasive cervical cancer if left untreated.
But how fast does this progression occur?
Let’s delve deeper into understanding the intricacies of CIN3 and its potential transition into cancer.
What is CIN?
Cervical Intraepithelial Neoplasia (CIN), also known as cervical dysplasia, is a condition that might turn into cancer of the cervix.
It’s caused by the Human Papilloma Virus (HPV), which is often found during screening tests like a Pap test or HPV test.
If CIN isn’t treated, it could become full-blown cervical cancer.
CIN is divided into three types based on what the cells look like under a microscope:
CIN1 is a minor case that includes warts in the genital area.
CIN2 is a bit more serious with moderate abnormal cell growth.
The most serious is CIN3, which includes heavy abnormal cell growth and a type of non-invasive cancer called carcinoma-in-situ (CIS).
CIN Levels and Their Connection to HPV and Cervical Cancer
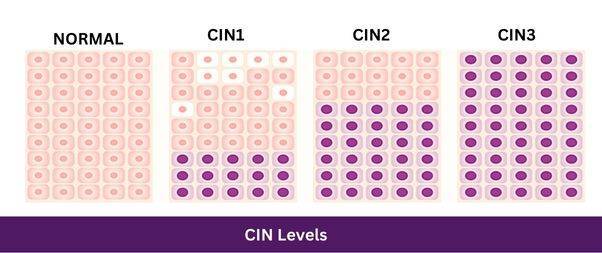
These are ranked based on how much of the skin layer of the cervix has abnormal cells growing.
CIN 1 is seen as low risk, with the abnormal cells in up to the bottom third of the skin layer.
CIN 2 and CIN 3 are high risk, with CIN 2 having the abnormal cells up to the top two thirds, and CIN 3 having them even further.
This condition and cervical cancer are caused by a sexually transmitted virus called HPV. This virus is quite common and up to 80% of women get it at some time in their life. Usually, the body clears the virus on its own, but sometimes it sticks around and can turn into CIN or even cancer.
In fact, HPV is found in over 99% of cervical cancer cases. It can also cause other cancers, like in the vulva, vagina, anus, back of the throat, and penis.
There are many types of HPV, but the most common types that cause genital warts are HPV 6 and 11. The most dangerous types, HPV 16 and 18, cause 70% of cervical cancers. Vaccines are available to prevent these types of HPV.
However, getting HPV doesn’t mean you’ll definitely get CIN. Most of the time, the immune system clears the virus within a year without any treatment needed.
Around 60% of CIN1 cases get better without treatment and less than 1% turn into cancer. But around 5% of CIN2 and 12% of CIN3 cases can become cancer if left untreated.
It usually takes 10 to 20 years for this to happen, which gives plenty of time to catch and treat it. Things like smoking, having HIV, and being immunosuppressed can make the HPV infection persist and the disease progress.
The same things that increase the risk for HPV and cervical cancer also increase the risk for CIN.
This includes starting sex at a young age, having multiple sexual partners, having a high-risk sexual partner, having other sexually transmitted infections, having abnormal cell growth in the vulva, vagina, or anus, being immunosuppressed, and smoking.
Usually, CIN 2 and 3 don’t have any symptoms and are found during a screening test. CIN 1 can lead to the development of genital warts.
The Pace of Progression
It’s crucial to understand that CIN3’s progression into invasive cervical cancer varies significantly among individuals, rendering it largely unpredictable.
This transition does not occur rapidly, but it’s also not negligible.
Cervical cancer is widely recognized as a slow-growing disease.
Studies indicate that if left untreated, approximately 30-50% of CIN3 lesions may progress to invasive cancer over a 30-year span.
However, this does not denote that CIN3 will inevitably evolve into cancer in every instance, nor does it prescribe a strict timeline.
The progression’s timeframe is influenced by several factors, including the individual’s immune response, age, overall health status, and the presence of high-risk HPV types.
Proactive Measures

When it comes to CIN 2 and CIN 3, most doctors recommend treatment because these conditions are less likely to get better on their own and more likely to turn into cancer.
Two types of treatment are often used:
- Ablative procedures
- Excisional procedures
Both are usually over 90% successful in properly selected patients.
Because of the potential for progression, the detection and treatment of CIN3 are instrumental in preventing cervical cancer.
Regular screening for cervical cancer, such as Pap smears and HPV testing, forms the cornerstone of this preventive approach.
These tests are particularly recommended for sexually active women and those aged 21 and over.
Should a CIN3 diagnosis be confirmed, there are several treatment options available, including
- Loop electrosurgical excision procedure (LEEP)
- Cold Knife Conization(CKC)
- Simple Hysterectomy
in specific circumstances.
The choice of treatment hinges on various factors, such as the woman’s age, the extent of the abnormal cells, and her desire to have children in the future.
Final Thoughts
Receiving a CIN3 diagnosis can be anxiety-inducing, especially with the associated risk of cervical cancer.
However, it’s important to remember that this condition does not guarantee a swift or definite progression to cancer.
Effective preventive measures and treatments are available.
Open conversations with healthcare providers about individual risk and appropriate screening measures are imperative.
These professionals can provide reassurance, guidance, and personalized care, turning the journey of CIN3 from a daunting diagnosis into a manageable health challenge.